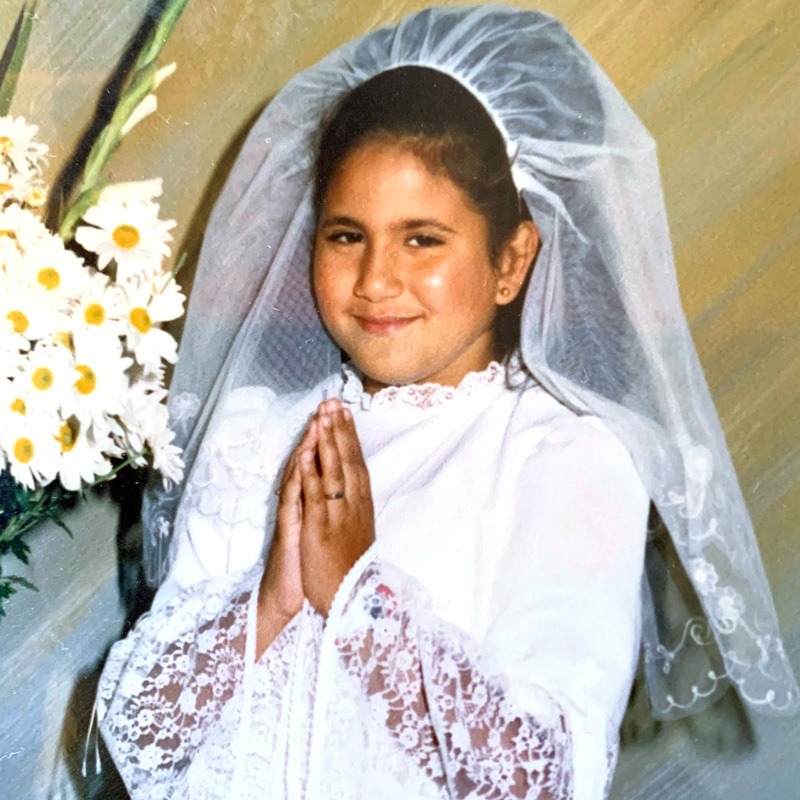
"I used to cry in fitting rooms," says 37-year-old Charmain Etnasios.
"I was always overweight - very uncomfortable with the way I looked, very self conscious."
In 2017, Charmain was, in medical terms, one of the 12.5 million Australians considered overweight or obese.
In Australia, significantly more men than women fall into this category. Recent research shows 71 per cent of men are overweight or obese, compared to 56 per cent of women.
It's women, however, who are more often than not the subject of the archetypal before and after photo: frowning on the left, in a larger body enveloped by larger clothes, and smiling on the right - a smaller frame meant to signify an unquestioned conduit to a better life.
Charmain has plenty of before and after photos. Just over two years ago, she underwent a sleeve gastrectomy - Australia's most common weight loss surgery.
But Charmain's story doesn't exist in a vacuum.
Out of every five people who opt for weight loss surgery in this country, four are women.
Beyond their before and afters are complex factors that have led to their decision to pursue surgery, as well as lived experiences that can't be captured with a camera.
Charmain tells Mamamia that ever since she was a child, shifting weight through diet and exercise had been a challenge. She’d grown up in a hospital chair next to her parents, both of whom had long, complicated medical histories. Then, at 21, a single moment upended her life.
On a Friday morning in January 2003, Charmain woke up to catch the train to Wollongong. She was meeting her boyfriend Hany, and everything that morning seemed to be going wrong. She missed her alarm, then rushed to Hurstville station, then had to call out to the conductor to open the train doors as she boarded at the last moment.
Fifteen minutes later, the train derailed, in an accident that killed seven.
“It was horrific. You’re lying there with blood all over you and people are dead. It was life- changing,” Charmain says.
She was left with seven fractured vertebrae, a fractured sternum, a torn ligament in her knee and a concussion.
Charmain explains that the ‘extra weight’ she was carrying didn’t help her compression fractures, and five years later, she developed Type 2 diabetes.
For years she battled with her weight, but she says that when she fell pregnant with her son at 32, she realised she didn’t want him to have the same life she had.
Throughout her pregnancy, Charmain had high blood pressure and sciatica, and her Type 2 diabetes meant she had extra medical care. She says she was eventually induced because of her health problems.
After giving birth to Nathaniel, Charmain was uncomfortable. She felt sluggish, got puffed easily, and while her friends lost their baby weight postpartum and started to feel better, Charmain didn’t. She’d been medically overweight for all her adult life and as a result had only gained 2kg during pregnancy - despite how much she felt her body had changed. This milestone was just another reminder that she wasn’t like other women. She wasn’t going to ‘bounce back’ like they did.
Despite her attempts to diet, the results were disheartening.
“I’d tell friends and family about a diet I was on, and they’d do it half heartedly and lose 20kg and I would be doing it for six months and only lose 3kg,” Charmain tells Mamamia.
To be eligible for weight loss surgery, you’re required to have a body mass index of more than 35, or 30 if you’ve got diabetes like Charmain. At the time of her surgery, her BMI was 38.
“Why can’t you lose weight on your own?”
“Weight is a bit like blood pressure. As we age, the body gradually increases its ‘set point’ for weight and this is a very powerful brain driver for hunger, because the brain registers the ‘set point’ as the highest weight the body has ever been,” explained Dr John Jorgensen, a bariatric surgeon at St George Private Hospital in Sydney.
“The bigger you are, the more powerful the hunger drivers. So when you’re 30-40kg overweight the excess weight is much much harder to lose. It’s biological, not anything to do with willpower,” he said.
“I was very uncomfortable with the way I looked," Charmain says of her wedding day.
Of course, not all medical professionals have this perspective when it comes to weight loss.
Annie, a 23-year-old from Orange, was told by her doctor that she “wasn’t trying hard enough” when she turned up to her GP time and time again, unable to drop any significant weight.
“I have always done sport and exercised 3-5 times a week. I ate fairly well. But nothing I seemed to do stopped the weight gain,” she explains to Mamamia.
“I tried all of the things; different diets, shakes, gym regimes - but I was never able to shift more than about 5kg.” Annie’s experience is the common one you’ll hear from weight loss surgery patients. Despite the widespread view that a person’s weight is within their control, for a great number of people, that doesn’t seem to be the case.
 Annie before and after her surgery. She has chosen not to reveal her full identity. Image supplied.
Annie before and after her surgery. She has chosen not to reveal her full identity. Image supplied.
While surgery is considered a last resort for patients who need to lose weight, Dr Jorgenson says there’s often no alternative that will see lasting results. “Many studies show that diet and exercise alone are hugely unsuccessful in very obese people with a success rate of 2-5 per cent long term,” he tells Mamamia.
Patricia Saran, a specialist bariatric nurse at the Sydney Institute For Obesity Surgery (SIOS), says there’s evidence of a genetic advantage to being unable to lose weight easily.
“People who have that ‘surviving’ gene can hold on to the energy they consume to make them be able to survive famine, wars, and desert conditions. They are designed to live and maintain no matter what their body is put through,” she explains to Mamamia.
“When you have the ‘obesity gene’, or prevalence [to put on weight] and we marry that with living in 2019 first world conditions where we are all doing very little and have access to highly calorific foods, that’s why we’ve got an obesity epidemic,” says Ms Saran.
Dr Jorgensen says obesity and diabetes are the “giant twin challenges” confronting the Australian health system, and while the Federal Government’s efforts to get people to exercise more and eat differently might help with mild weight loss, it’s “completely failing on the obesity front, where hunger drivers are just too powerful.”
“Surgery helps to reset the brain’s weight set point and hunger drivers. Many people come to hospital with diabetes and walk away without it.
“Many people perceive surgery as a cosmetic type procedure, but really it is about saving lives,” says Dr Jorgensen.
What does surgery look like?
While there are a number of different types of weight loss surgery a patient can opt for, the most common, and the one recommended to Charmain, is the sleeve gastrectomy or “gastric sleeve”.
With private health insurance, the procedure cost Charmain $8,500. Without insurance, she would have paid close to $23,000. Currently, the Australian and New Zealand Metabolic and Obesity Surgery Society is trying to lobby the government to improve access to these types of surgeries - citing that 67 per cent of Australian adults are overweight or obese. They say greater access to weight loss procedures will save lives and money.
During the gastric sleeve procedure, a surgeon reduces a patient’s stomach to about 15 per cent of its original size. It’s done via keyhole surgery, takes about two hours, and involves a stapling device that creates the new smaller sleeve shaped stomach before cutting away the rest of it.
At the Sydney Institute for Obesity Surgery, patients are given a program of pre-operative assessments. “They’ll see a psychologist to make sure there’s no underlying concerns and are worked up by the whole team. We also have our own GP assess them. Post surgery there’s the dietician, surgical team and psychotherapy if needed,” said Ms Saran.
But that isn’t mandatory. A surgeon doesn’t have to offer all of these extras, it’s just advised. For example Charmain saw a dietician, but she opted not to see a psychologist.
On the day of surgery, Charmain was terrified. “I was shaking and saying ‘I can’t do this I want to go home’ and I was so nervous they had to give me something to calm me down,” she told Mamamia.
Waking up afterwards she felt sick and nauseous and had a “stretchy” feeling in her stomach. “I had a hard recovery, most people leave on day two but I was there for five days. I felt so restricted, I couldn’t fit anything in [to my stomach] and I needed to be doing two litres of water a day otherwise I couldn’t go home."
Sydney woman Carol was also in hospital for four nights, but admits “she was up going to the bathroom within four hours of surgery.”
She realised firsthand just how differently the surgery hits everyone. “I met with all of the people at my hospital who’d had the same surgery in the past 48 hours. Each one of us had a very different post-op experience. Some had woken up in extreme pain, others said they could have gone for a 12km run. One guy asked how quickly he could play golf, another said it was more painful than childbirth,” she said.
Post surgery, patients are put on a two week ‘diet,’ which Charmain says she found unpleasant. It consists of soups, shakes and not much else.
Carol, who only had her surgery a few months ago, tells Mamamia she quite liked the liquid diet she was required to follow.
“I had shakes for breakfast, lunch and dinner, and they tasted amazing. There’s five different flavours; chocolate, honeycomb, vanilla…” she said, adding that she found the liquid diet crucial in teaching her body and mind not to think about food like she used to.
But for some, adjusting to new portions post surgery is intensely difficult.
“My first meal out with friends after surgery I overate, and I started to withdraw from conversation because I was so uncomfortable,” Charmain said. “I had to go the bathroom and vomit. It’s a discomfort that sits in the top of your stomach..it feels like you’ve eaten a whole cow [after only a few bites] and it just sits there for an hour and a half.
"I couldn't even fit a Petit Miam yoghurt in in one go."
Does it work?
Everyone loses weight after having weight loss surgery.
Current research shows that bariatric procedures result in more significant weight loss, both in the short and long-term, than any other method.
After surgery, a majority of weight loss tends to occur in the first year, and decreases moderately over time.
There's a need for more research on the long-term outcomes of bariatric procedures, but the available evidence suggests the majority of patients will maintain most of their weight loss over a period of 10+ years.
There are, however, exceptions to that rule.
Libby Oakes Ash is one woman who regained weight after surgery. The Canberra woman went public with her story last year, and was inundated by messages from 30 women who were grateful their side of the weight loss surgery story was finally being told.
“A lot of these women all had the same story as me, in that the first 2-3 years is the ‘honeymoon period’,” she told Mamamia. “You can’t put on weight because you cannot eat and your stomach [has shrunk to a point] that when you do overeat, you vomit.”
“The hunger hormone disappears after surgery but it comes back - they don’t tell you that. It comes back insidiously,” she said.
Charmain’s ‘hunger hormone’ kicked in a lot quicker than she was warned. Hers was back within three months and she says when it did, that’s when it got really hard.
“I’d be sitting on the couch with Nathaniel and he’d be watching Thomas and Friends and I’d seriously be thinking “mmm pizza, pasta, BBQ chicken”, it was terrible. Your brain wants to eat it but you know you can’t because you’ll be sick.”
“Sometimes I’d try and sleep at like 8.30pm so I wouldn’t feel the brain hunger.”
The stomach eventually starts to stretch back out again after time, which is something Ms Saran confirmed to Mamamia. “Think about how babies grow, their stomachs are tiny when they’re born but they grow. Or think about how a pregnant woman’s stomach stretches over time,” she said. “It’s the same concept.”
Libby, who had her surgery in 2015, went from eating half a sandwich in the first year, to being able to eat a whole sandwich by the second year, until eventually she was essentially back to normal portion sizes. “I have started to put on weight again...I’ve put 19kg back on,” she told Mamamia.
“I also lost masses of my hair and started to go bald in patches on my head. Every woman I’ve spoken to has gone through that too...and their nails have gone brittle.”
For Libby, trying to lose weight now, years after having her surgery, is harder than it's ever been. Nonetheless, she continues to work on getting the weight off by eating well and exercising.
"Once you put weight back on, it seems twice as hard to get it off," she explained. "[It's] like your body is fighting you."
Below are photos of Libby throughout her surgery journey.

Then, of course, there’s the psychological and emotional impact.
Ten months post surgery, Sydney-based Maria* is now suffering from an eating disorder characterised by restrictive eating and body dysmorphia.
“I was told people who have an eating disorder have some kind of dormant gene and that it can be triggered. For me losing the rapid weight (I’ve lost 47kg) was the trigger,” she told Mamamia.
“My mind hasn’t caught up to where my body is at. I can’t see any difference. If I was to do before and after photos, everyone tells me I look so different and skinny, and I end up hating that. It grinds me the wrong way because I don’t see that,” she said.
Phillipa Hay is a psychiatrist who specialises in eating disorders, and is used to seeing patients who have developed psychological issues after having weight loss surgery.
“It’s becoming increasingly common. It’s usually to do with difficulties stopping the weight loss. Patients can develop an anorexia nervosa type problem,” she said.
“They’re suddenly getting endorsements because of their weight loss and there’s often an increase in feelings of self worth and self regard… it has an impact on their mental health and interpersonal relationships,” she said.
These endorsements based on physical appearance are a phenomenon the Health at Every Size movement has long recognised as problematic. “Congratulating a human for changing the size or shape of their body sends the message that their worth as a person depends on their physical form,” said HAES dietician and nutritionist Mandy-Lee Noble.
“A person’s physical appearance tells you nothing about how they are feeling and their mental health.”
For Maria, her rapid weight loss made her “afraid to eat”.
“Putting on weight again became a huge fear,” she said.
Other patients, however, feel overwhelmingly positive about their decision.
Speaking to Mamamia, Queensland mum Sophie* says “this surgery saved my life”.
“I had the sleeve in December 2016 and if I had to, I would do it all over again. I’ve lost 64kg over this time. I thought I was happy before, but it’s not until you see how much your weight was impacting every facet of your life that you realise how desperately unhappy you were.”
Charmain smiles when she speaks about how the surgery has changed her.
“My diabetes is gone, I am so much healthier, I am comfortable in my skin, and I can run after my son. Everything is so much better,” she told Mamamia.
What's missing in the weight loss surgery conversation
In her work as a dietitian, Mandy-Lee Noble sees significant gaps in the framework surrounding weight loss surgery.
“I’ve had clients report on-going gastrointestinal problems, weight regain, and increased alcohol use,” Ms Noble told Mamamia. “People who consider bariatric surgery need to be fully informed.”
Lauren* put all her weight back on after her gastric sleeve procedure because she had reflux post surgery, which would flare up when her stomach was empty. She was so disappointed when she, as a result, put the kilos back on.
“I was very open with friends and family about having the sleeve but haven’t been so open since because I feel like a failure,” she told Mamamia.
For Ms Noble, a significant issue lies with the fact that while surgery achieves weight loss, it does nothing for weight stigma.
“Portraying drastic weight loss stories as heroic is corrosive to the mental and physical health of people in larger bodies and reinforces the belief that people in bigger bodies need to be seen as ‘good fatties’ (ie, trying to lose weight at all times) in order to be acceptable,” she said.
The resounding statistic that 80 per cent of those who opt for weight loss surgery are women tells a story in itself.
Professor Hay argues that these numbers are tied to the fact that as women, we’re so obsessed with body shape, and the ‘ideal’ thin, toned female figure we’re ‘supposed’ to be striving for.
“Patients might be doing it for medical reasons, and the surgeons are certainly doing it for medical reasons - but eating, body shape and weight are all very connected in terms of the overall psychological view of yourself. So that can’t be discounted even if it’s not the primary reason people put forward as their ‘reason’ for surgery,” she says.
Ms Noble agrees. “No one talks about the fact that weight loss surgery is gender driven,” she says, “which is a strong indicator that the pressure on women to conform to social norms around body size and shape influences their decision to have surgery.”
While her diabetes, parent’s medical history and the compression fractures she suffered in the Waterfall train disaster (which she feared would get worse the more weight she carried) were Charmain’s main reasons for surgery, she also admits there was a cosmetic element.
“I was very uncomfortable with the way I looked, I was very self conscious,” she said. “I wish my wedding photos didn’t look the way they look.”
“Nathaniel does swimming lessons and I have to get in the pool with him. I probably wouldn’t have enrolled in swimming lessons if I was [still] overweight and I know that sounds terrible but I would’ve been too embarrassed to get in the pool. Or I would have done it on a weekend when Hany could take him,” she said.
“I used to cry in fitting rooms because I’d go into a standard shop like Target and they wouldn’t have a size that fit me,” she said. “And in summer, I would avoid the beach. I’d always just say ‘let’s go to my brother’s pool’ because there’d be no public people who could see me there.”
It’s been just over two years since Charmain’s surgery, and while she worries about weight regain, she’s confident in her post-surgery plan.
She’s currently within the BMI range considered ‘healthy’ by medical professionals, and the changes to her body mean she’s able to run after her three-year-old without having to stop and catch her breath.
But not every story ends like Charmain’s.
There are women like Libby, who put weight back on, or Maria, who now has an eating disorder triggered by her surgery.
There are the women who didn't want to talk to Mamamia about their experience, because they felt they weren't given the ending they were promised.
And for all these women - the four in five who opt for weight loss surgery - their decision can’t be separated from the complex world in which they live. Eating, body shape and weight are uniquely tied to women’s identities, and it’s undeniable that these factors, as well as the pursuit of health, lead them to the operating table.
These women can't be reduced to before and after photos, as though their bodies are where their stories begin and end.
Reporting
Gemma Bath
Design
Millie Carter
Development
Paul Sharratt, James McGrath & Meghna Narayanan
Editor
Clare Stephens
For more from Gemma Bath, you can subscribe to her weekly newsletter.